May is Maternal Mental Health Awareness Month. There are several organizations, like Postpartum Support International, coming together during this month to remove the stigma of mental health issues in mothers so that more people can have access to help and care. Maternal mental health conditions are treatable, however many new and new again moms do not seek out help for a variety of reasons. Maybe there is a stigma around seeking help. Maybe you are scared of the thoughts that you are having about your baby. Or maybe the needs of others and caring for family leave you with little time for yourself. You are not alone in these concerns and help is possible.
It is estimated that 20% of women in the perinatal time frame will experience a Perinatal Mood and Anxiety Disorder (PMAD). This means that 1 in 5 women experience symptoms of depression, anxiety, post-traumatic stress, or obsessive-compulsive thoughts and behaviors in the perinatal time frame which includes pregnancy through 12 months after giving birth (Postpartum Support International, 2023).
Fathers and partners can also experience depression within the postpartum period with an estimated 10% reporting symptoms of depression (PSI, 2023).
You might be asking, how do I know when I need help for my mental health concerns? Aren’t emotional ups and downs a normal part of pregnancy and the first year of motherhood?
While “baby blues” or postpartum reactivity are very common in the perinatal period, there is a difference between postpartum reactivity and a perinatal mental health concern that needs more attention and possible help from therapists and doctors.
What are the major differences between Postpartum Depression & ‘Baby Blues’?
Postpartum reactivity is characterized by tearfulness, exhaustion, and emotional reactivity. One main cause is the dramatic changes and fluctuation in hormones in the weeks after giving birth. Lack of sleep is also a major contributing factor. These “baby blues” universally affect about 80% of postpartum women. The main distinguishing factor is that this condition usually resolves on its own within the first few weeks postpartum (Manzella, 2022).
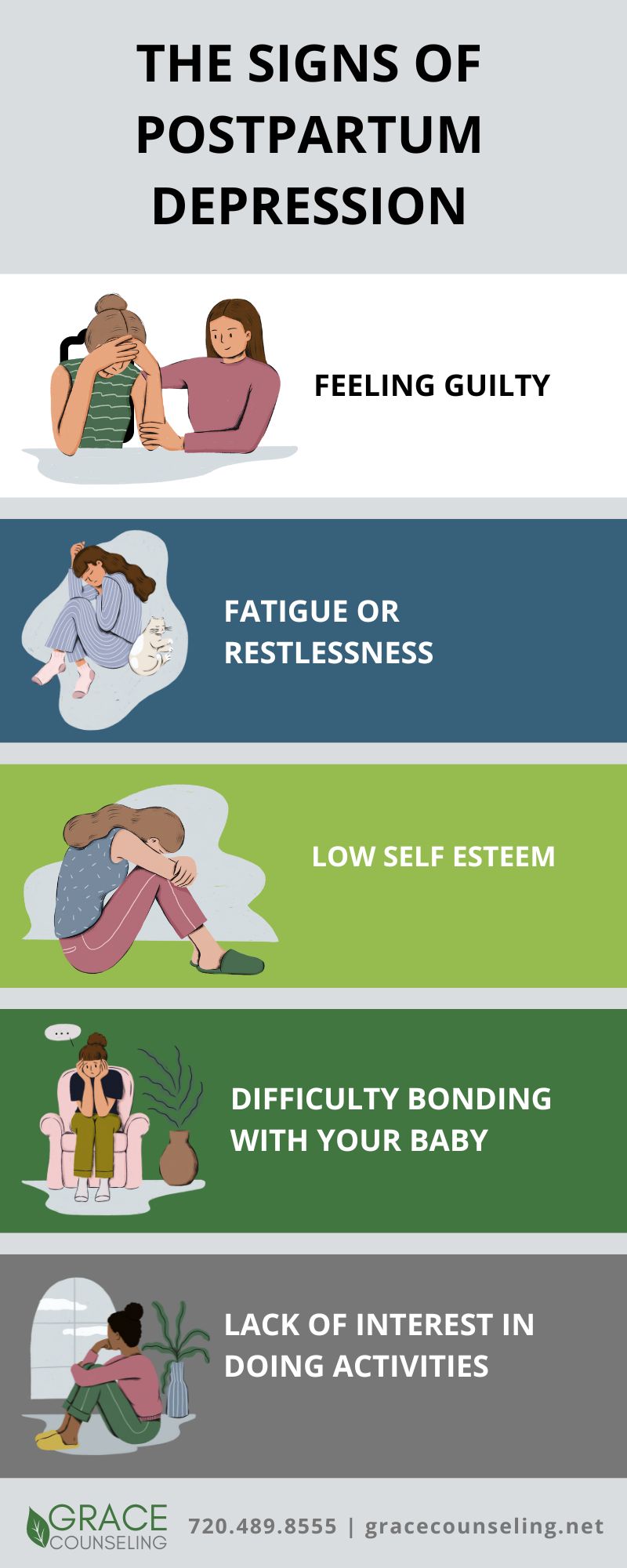
In contrast, a PMAD will last longer in the postpartum period and can begin to develop during pregnancy as well. Postpartum depression is characterized by feeling sad, guilty, or angry, being more irritable, having difficulties sleeping or eating, having difficulties bonding with the baby, and having negative intrusive thoughts. One main difference to watch out for between “baby blues” and postpartum depression is self-esteem. In “baby blues,” a woman’s sense of self and self-esteem remain the same, while a woman experiencing postpartum depression will
have lower self-esteem and more negative thoughts about herself (Manzella, 2022).
– Written by Danica Hungerford, MA, LPC
 Postpartum Support in South Denver
Postpartum Support in South Denver
If you are feeling overwhelmed, emotionally drained, or wonder if you are experiencing postpartum depression or another PMAD, you do not have to suffer in silence. Help and support can be found through therapy, support groups, or through medical help from your doctor. You can also find more resources through the Postpartum Support International website. You are not alone, and you can experience joy again.
Call today to schedule an in-person or virtual appointment with Danica, or one of our maternal health professionals here at Grace Counseling in South Denver.
References
Manzella, C. (2022). The Maternal mental health intensive: Perinatal mood and anxiety disorders. [Online Lecture]. Seleni Institute.
Postpartum Support International. (2023, April). Parents Fact Sheet.



 Postpartum Support in South Denver
Postpartum Support in South Denver


Leave A Comment